
Nearly four years ago, Becca Brown, a 41-year-old resident of Burlington, Vermont, noticed a grape-size lump on the side of her breast as she was getting ready for bed. Follow-up testing revealed a fast-spreading cancer, but its early detection meant the tumor responded better to treatment, and ultimately, Brown recovered from the disease.
"Even if you find something little, you've got to go in and get it checked out," Brown told Live Science, relaying advice she would give other people. "And it's important to know your 'breast baseline' so you can tell if something is out of the ordinary," she added.
Experts used to recommend that people at average risk of breast cancer conduct breast self-exams, which would involve regularly checking their breasts by sight and by touch for any notable changes. These checks, which follow a specific procedure, were widely encouraged in breast-cancer awareness campaigns, as well.
So should you check yourself for breast cancer? Nowadays, doctors actually advocate for something a bit less structured than self-checks — what they call "breast self-awareness." This means being generally attuned to what your breasts look and feel like, rather than doing formal self-examinations.
Here's why the recommendations changed and what experts now recommend you do instead.
Related: Does it matter what time of day you get cancer treatment?
The shift from breast self-exams to self-awareness
Many women detect their own breast cancers, with an estimated 25% uncovering tumors by deliberate self-examination and 18% doing so by accident, according to a 2011 study published in the Journal of Women's Health.
Nonetheless, breast self-exams are no longer recommended in women who are at average risk of breast cancer, meaning their risk isn't heightened by genetics or family history, for example. That call was made by leading experts in the field, including the U.S. Preventive Services Task Force, the American Cancer Society, and the American College of Obstetricians and Gynecologists.
Research has found that breast self-exams have led to a higher rate of people getting tested for cancer via imaging and biopsies and getting false positives, meaning tests suggested they had cancer but they actually didn't.
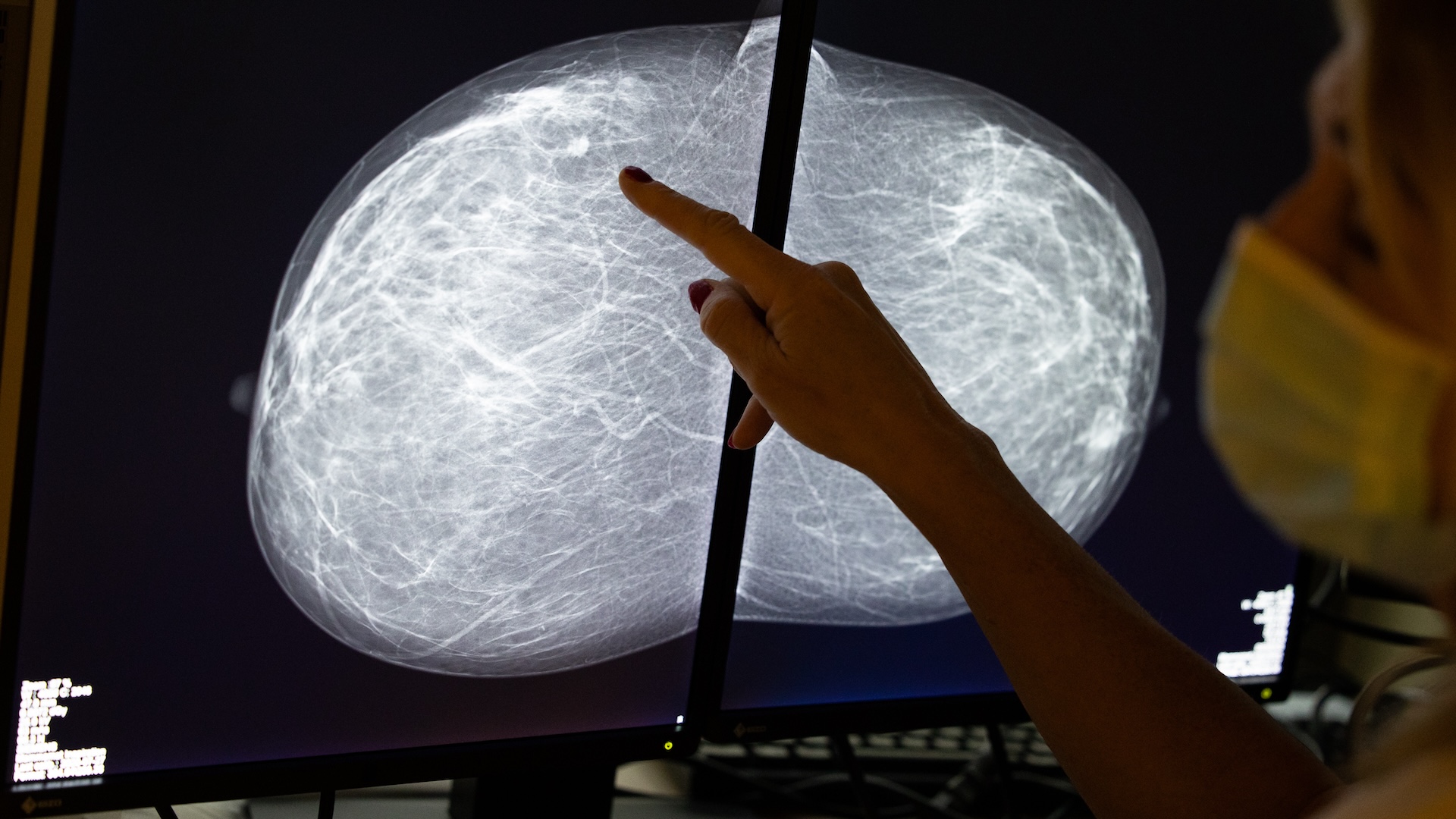
Simultaneously, this increase in testing didn't come with an increase in early diagnoses or a reduction in cancer deaths, according to a study in the Journal of the National Cancer Institute. These types of benefits are associated with other screening methods, such as mammograms. Importantly, the goal of any screening is to detect signs of cancer early and flag a person for follow-up testing, where a formal diagnosis may then be made.
In light of these findings, experts shifted their recommendations. Instead, they now encourage patients to just tune into the usual appearance and feel of their breasts.
Related:Black patients may need breast cancer screenings earlier than what many guidelines recommend
Unlike self-checks, these aren't systematic examinations of the breast tissue. "It's not a doing; it's more of a knowing," Dr. Mary Gemignani, chief breast cancer surgeon at NYU Langone Health, told Live Science. "Most women know their bodies better than providers do, and any changes should be reported." Breast exams conducted by doctors are also not recommended for breast cancer screening anymore.
On an individual level, however, some doctors argue that any form of self-screening — whether a formal self-exam or simply self-awareness — has benefits that outweigh the risk of false positives and unnecessary testing.
"There are false positives and angst and anxiety that go into this, but I think most people are OK with that," said Dr. Mehra Golshan, deputy chief medical officer for surgical services at Smilow Cancer Hospital and Yale Cancer Center in New Haven, Connecticut. Many patients would rather be safe than sorry. "It's a good phone call to receive that your result was benign," he said.
Most changes found through a self-exam or self-awareness end up being harmless, Golshan said. But he added that, anecdotally, several patients at his practice have identified cancers that were missed by routine imaging.
How to practice breast self-awareness, and when to get screened
Practicing self-awareness means regularly taking notice of how your breasts look and feel, perhaps when you're in the shower or getting dressed.
Gemignani said changes to look out for might include lumps on the breast, hardening of the breast tissue, skin discoloration or changes in the lymph nodes, which could cause swelling in the armpits or around the collarbone. Also look out for inverted nipples and nipple discharge. New asymmetry in the breasts' overall shape or a noticeable change in one breast relative to the other may also warrant follow-up testing, Gemignani added.
Breast self-awareness should not replace other breast cancer screening methods, such as mammography and magnetic resonance imaging (MRI), doctors caution. Self-awareness should be practiced between these regular screenings so that any changes detected can be quickly brought to a doctor's attention.
There are subtle differences in how often different groups advise patients to get screened. The U.S. Preventive Services Task Force recommends that female patients ages 40 to 74 who are at average risk of breast cancer get a mammogram every two years. The American College of Gynecologists and Obstetricians recommends that screening begin at age 40 and be repeated every one to two years until age 75. Meanwhile, the American Cancer Society suggests annual mammograms for people ages 45 to 54 and then mammograms every other year after age 55.
Some people may benefit from starting screening at younger ages or from getting different screening methods, depending on their family history of cancer and their genetics, Gemignani said. Having dense breasts, a mother or grandmother with breast cancer, or a family history of ovarian cancer can put you in a higher risk category that requires earlier or more frequent screening.
Gemignani advises people with a strong family history of relevant cancers to speak with their gynecologists and consider genetic counseling to better understand their own risk. A genetic test can identify changes within certain genes, such as the BRCA1 and BRCA2 genes that are linked to a higher risk of breast cancer.
Brown emphasized that it is critical that any changes detected with breast self-awareness — no matter how small they may seem — be brought to a doctor's attention to rule out cancer or identify the disease early.
"It's not enough to just find the lump," Brown said. "You actually have to go get it checked out and take action."
This article is for informational purposes only and is not meant to offer medical advice.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!







