The last thing Melbourne mum Annie O'Brien did before she died was miscarry her second child.
The 37-year-old died from multi-organ failure caused by a sepsis infection within hours of delivering her baby at 18 weeks, and less than 24 hours after falling ill in August 2017.
An inquest found deficiencies in the care given at two Melbourne private hospitals to Ms O'Brien, the mother of a 14-month-old son and partner in a law firm.
State Coroner John Cain made no formal findings about the nursing or medical management she received at the Holmesglen Private Hospital or St Vincent's Hospital, but noted clear evidence of deficiencies in the care provided to her.
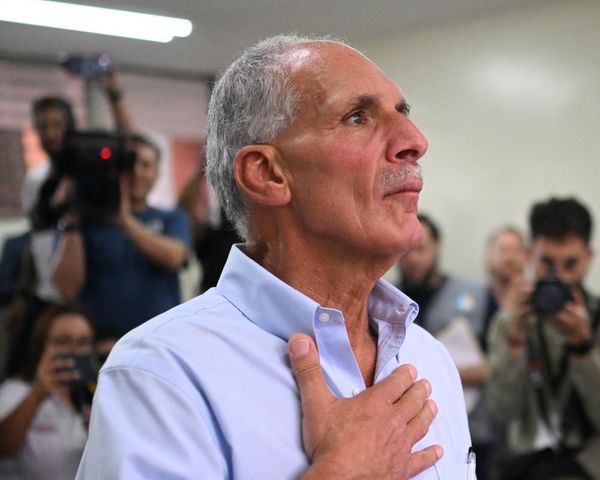
Ms O'Brien's parents, Brian and Marg Moylan, want a full review of private and public health services in Victoria, a yearly audit into critical incidents in public hospitals, and to make Victorians aware of the standard of care they should expect.
"The clinical aspects were critical in Annie's case. Her care was dreadful ... she had a right to expect much more," Dr Moylan, a retired GP, said.
"In our view, her death was preventable and with reasonable systems of care, with reasonable clinical judgment, she would be alive today, her baby would be alive today."
Dr Moylan said his daughter would "want a legacy of change above all else".
Medical experts gave widely varying opinions on whether Ms O'Brien could have survived if given antibiotics at any stage of her treatment, but Judge Cain concluded her greatest chance for survival would have been if she had been given them by 8.30pm on August 14.
By 10.15pm, when her condition deteriorated, there was nothing that could have been done to prevent her death, he said.
Ms O'Brien had only fallen ill after lunch that day, leaving work early with gastroenteritis symptoms. An obstetrician prescribed rest and paracetamol.
That evening she called her dad to say she needed to go to hospital.
She was triaged at Holmesglen Private Hospital to be seen within 30 minutes but waited more than an hour for Hui Li Shi, the sole doctor in charge of the 10-bed emergency department.
She was diagnosed with gastro and given fluids. By 9.30pm she felt better and wanted to go home. Within 45 minutes she was critically unwell.
It's at that point sepsis became a diagnosis that needed to be excluded, Judge Cain said. Dr Shi should have reconsidered her gastro diagnosis, but did not, he said.
Dr Shi had told the inquest she wasn't aware of the hospital's sepsis guidelines, but regardless Judge Cain said as an emergency physician she should be expected to be aware of the signs and symptoms.
The doctor arranged for Ms O'Brien to be transferred to St Vincent's and be met by obstetrician, Vicki Nott.
Dr Shi claimed she told Dr Nott about the urgency, but Dr Nott said she didn't know it was a medical emergency.
At 12.40am, midwife Gillian Codd called Dr Nott to express concerns about the seriousness of Ms O'Brien's condition.
Dr Nott should have ordered antibiotics then, Judge Cain said.
She didn't arrive at the hospital for another 50 minutes, then sat in her car for 10 minutes researching antibiotics. She should have known what to give, Judge Cain said.
After giving sepsis as a possible diagnosis at 1.45am, Dr Nott disappeared for 20 minutes searching for sepsis guidelines.
A prescription was written at 2am and Ms O'Brien got her first dose at 2.46am after midwife Raechel Miller spotted the medication on a table.
Judge Cain commended the midwives for their care.
Ms O'Brien's life support was turned off at 1.55pm on August 15.
Judge Cain has recommended Victoria's health department mandate root cause analysis reports of serious adverse patient events in all health facilities, public and private.
He has also asked Safer Care Victoria consider including a section on maternal sepsis and antibiotics in their guidelines.