As a young woman of forty-four, menopause hadn’t even entered my vocabulary. I was slightly cocky about the fact that I thought I could easily crack out another couple of kids (even though I didn’t want to... talk about the arrogance of youth), so when it did happen, the perimenopause (again, a completely new concept to me) not only crept up on me but hit me like a train.
I wasn’t prepared for it. I didn’t even realise it was happening. And yet fast forward a few years and I’ve co-written a whole book about it. A book that went on to win Best Book of the Year at the British Book Awards.
Nothing has surprised me more. Not least because, sitting at that awards ceremony, I really didn’t feel like an author – I felt like a fake being there. But if a book about menopause can be chosen above literally thousands of other absolutely brilliant books to be recognised in that way, it tells us a lot about how much a guide to this phase of our life was – and still is – urgently needed.
There were lots of things that I wanted to do with Menopausing. I wanted it to be a really easy book to use. I wanted to put important things in big type on single pages, so that something would jump out at you and you’d go, "Oh, hang on, I’m going to stop here. I need to read that."
So many women – and men – still contact me with really touching messages about how the book has helped them, saying it struck a chord, and most importantly that it’s enabled them to find their stride and thrive at this stage of their life.
Luckily, conversations are continuing and changes are happening. The first edition of the book was published in 2022 and, from 2021 to 2022, 7.8 million items for hormone replacement therapy (HRT) were prescribed, a 35% increase from 2020 to 2021.
Then, from 2022 to 2023, 11 million items were prescribed, another 47% increase from 2021 to 2022. That truly is amazing because it suggests that word is getting out there and that the stigmas and misinformation around HRT are dissipating and women who can and want to take it are choosing to do so, and they’re able to access it.
And yet, while that is a big difference, it’s not enough. Socioeconomically, HRT usage is still heavily weighted towards the wealthy, and areas of greater deprivation in the UK have the lowest number of women being prescribed HRT. Why? Why is there still that barrier to access?
Pushing for workplace menopause strategies
Another brilliant step forward and something that I found really heartwarming is that lots and lots of businesses are getting really robust menopause strategies in place. I’ve done lots of talks in companies that are implementing different types of women’s health resources, such as menopause champions, flexible working, additional training or inviting a healthcare professional who is an expert in menopause or in women’s health issues to come into the workplace twice a month and women can get an appointment with them.
If you’re reading this, and changes aren’t being made in your company to support you, then suggest it. And to any business owners, please, please do the right thing. Feeling supported keeps your workforce happy and keeps it working more efficiently and that’s got to be a good thing for your business. You need your older women, you need their experience, and you need their talent, so please stop ignoring them and set up processes and strategies to respond to their needs. Otherwise, you’re going to lose them.
Overmedicalisation or steps forward?
In this country particularly, we educate, educate, educate, then progress is made and there’s a reaction or a backlash to that progress. There are amazing doctors and other celebrities doing brilliant things and using their platforms to get information about perimenopause and menopause out there, but somehow that education and empowerment seems to make people in certain camps nervous.
Plus, in the past year, there have been articles talking about the "overmedicalisation" of menopause, saying that most women should navigate menopause without the need for treatment and further, that overmedicalisation can lead to the disempowerment of women, presenting a negative picture of this point in our life.
What does it mean to say it’s over-medicalised? Why is making ourselves feel better a bad thing? We can’t sidestep the menopause. Roughly 75% of women will have some kind of symptoms ranging from slightly annoying to potentially life-threatening. And while it’s a relatively small amount of people that find it life-threatening, around 25% will find it incredibly debilitating and around 50% will find it a bit annoying.
I’m in this group and I really needed support and education to get myself through it. And when I did get myself to a better place with it, I thought, my god, other women need this information and this support, too. It can be a tricky period in our lives but if we have the information to understand it and make choices about how to cope with it, it’s easier.
What’s so, so sad about these claims of overmedicalisation is that they shame or embarrass women into not taking HRT. Women who might already be nervous about starting to take HRT are being made to feel worse for even contemplating it. To be made to believe you’re a weak person for wanting to help yourself feel better, or you’re going against nature, makes me really, really sad.
Because I know how this point in your life can feel. I know how lonely it can feel. And the fact is that taking HRT can really help you find the joy in your life again.
I’m not pushing HRT. I’m a massive advocate of freedom of choice - I want to educate, support and inform women to allow them to make their own choices. I just want to reframe the way that HRT is viewed by society because the more we talk about it, the less shameful it becomes. I want to demystify it so that women can decide whether to take it or not, based on facts rather than scaremongering or misinformation.
Encouraging open conversation
I wish we could all have an open discussion without arguing with each other and without organisations that deal with women’s health shaming us for a period in our lives that can be helped with medication if we need it. And I count myself as one of those people – I really needed it. And if women don’t want to take it – great. I just want us all to come together and talk about it sensibly, with an option for the women that really need it; an option for the women that can’t take it; and support for the women that don’t want to take it.
What I’d really love is for important groups, such as the British Medical Society (BMS), which does a brilliant job of educating the medical field, and the Faculty of Sexual and Reproductive Healthcare (FSRH), to use celebrities and other people with platforms. We want to help you get your message out there. Use us as amplifiers.
My menopause mission
In 2021, my documentary Sex, Myths and the Menopause – which lifted the lid on misinformation surrounding the menopause and examined the science and fear around hormone replacement therapy – aired on Channel 4. In the days that followed, something really unexpected and amazing happened. I have never ever presented a show that’s made so many people want to stop me in the street to talk about it. Not even Big Brother.
People spoke to me everywhere I went - on dog walks, in the supermarket, and just walking down the street. Some women were in tears sharing their stories of feeling invisible, marginalised and patronised. Some men and women telling me how much they'd enjoyed watching it with their partners, and how it had given them a better understanding of what their loved ones were going through. It was totally and beautifully overwhelming.
Those moments lit a fire in me and made me feel like I needed to do more – to reach more women. I don’t want women – or men – to hear about menopause from friends who are going through it. I would like every woman to know about perimenopause and menopause by the age of thirty, at least, so that they're prepared for it and are armed with the knowledge to face it head on.
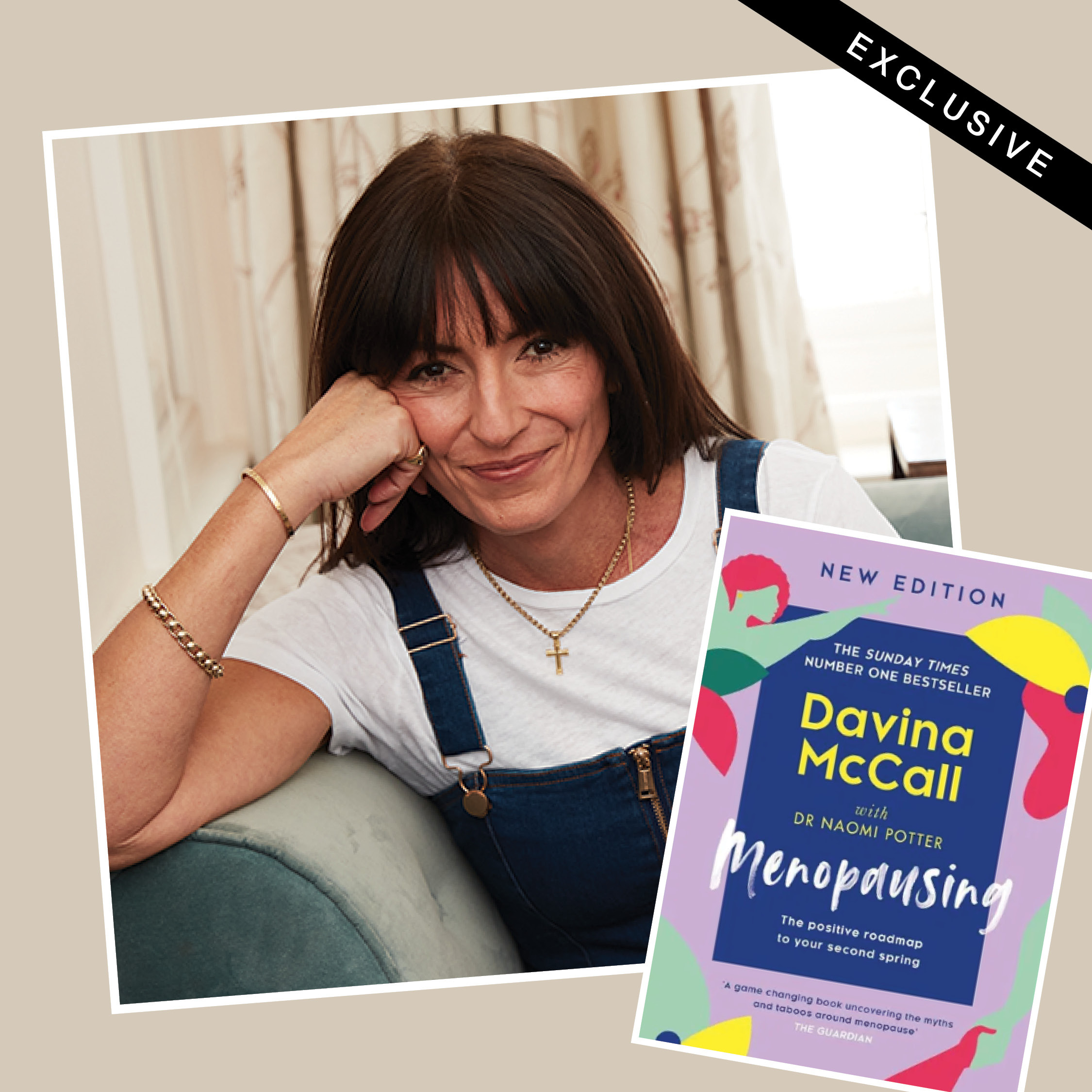
The revised edition of Menopausing, by Davina McCall and Dr Naomi Potter, is out today. It's been updated to reflect the changes in the conversation around menopause and the treatments available, exploring and explaining the science and smashing the taboos related to perimenopause and menopause.







