In May 2021, Australia’s chief medical officer, Prof Paul Kelly, described how Covid vaccines were our “ticket out of the pandemic”. Vaccination, he said, would give Australians “a life with more certainty”.
More than one year later, Australia’s Covid-19 vaccination rate is among the highest in the world.
Yet daily deaths from the virus remain in the double-digits. Hospitals are overwhelmed, aged care homes and the most vulnerable are struggling with outbreaks, and there is again debate about whether more social restrictions, including mask mandates, are needed to curb virus spread.
Infectious diseases expert and director of the Doherty Institute, Prof Sharon Lewin, said: “Last year, I definitely did not think we would be in this position.”
“I definitely thought that with very high vaccination rates and what we knew about Covid vaccination and protection against disease from other variants, it would put us in very good stead.
“But I think what we’ve learned, especially over the last four-to-six weeks here in Australia, is the virus really does have a lot of new tricks that were unanticipated.”
Its latest trick is Omicron, a variant that has produced the subvariants BA.4 and BA.5, which are now dominating new infections in most parts of the world.
These variants are immune evasive; whether that immunity comes from vaccination, or infection from other variants and subvariants. They are also highly infectious; between 10-to-20 times more so, Lewin says, than the original strain first identified in Wuhan, China, in late 2019.
“BA.4 and BA.5 are so infectious, that those infections are very hard to control because they are just so large in number,” she said.
“The infectiousness of Omicron and the limited capacity for vaccines to protect against infection [though they do protect against severe disease and death], means you’ve got high case numbers, which has a big impact on how society functions. This includes the impact on the healthcare workforce, on our transport workforce, and all the sorts of industries we need just to run the country.
“Even if it’s just a very small percentage of those that end up in hospital, it’s still a large number overall, and the same is true with regard to long Covid which may potentially gives us a big burden of disease over time.
“It’s this evolution of the virus in this way which has surprised virologists, evolutionary biologists, and vaccinologists.”
‘We should expect more variants’
Part of the reason variants like Omicron emerged so rapidly is because of the uncontrolled spread of the virus in vulnerable populations. People with weakened immune systems are more likely to remain infected with Covid-19 for several weeks or months, increasing the virus’s opportunity to mutate.
These prolonged infections have been seen particularly in patients with advanced, untreated HIV – a serious problem in sub-Saharan Africa, where the Omicron variant was first detected in November, thanks to the continent’s strong surveillance systems.
In an opinion piece for Nature magazine, researchers argued that vaccine equity – along with access to treatment for HIV in Africa and curbing stigma – could help the world see fewer Covid variants emerge.
In January 2021, WHO director general Dr Tedros Adhanom Ghebreyesus warned “the world is on the brink of a catastrophic moral failure – and the price of this failure will be paid with lives and livelihoods in the world’s poorest countries”.
He expressed concern that high-income countries were acquiring the bulk of vaccines, while other countries were being left behind.
“Not only does this me-first approach leave the world’s poorest and most vulnerable people at risk, it’s also self-defeating,” he said. “Ultimately, these actions will only prolong the pandemic, the restrictions needed to contain it, and human and economic suffering.”
Prof Penny Moore, a virologist with the National Institute for Communicable Diseases in South Africa, said it is not just a lack of protection for vulnerable immunocompromised people – many of whom don’t even realise they’ve been infected with Covid because they’re asymptomatic – and a lack of equitable access to healthcare including vaccines, and antivirals for HIV and Covid-19 that are a problem in her country.
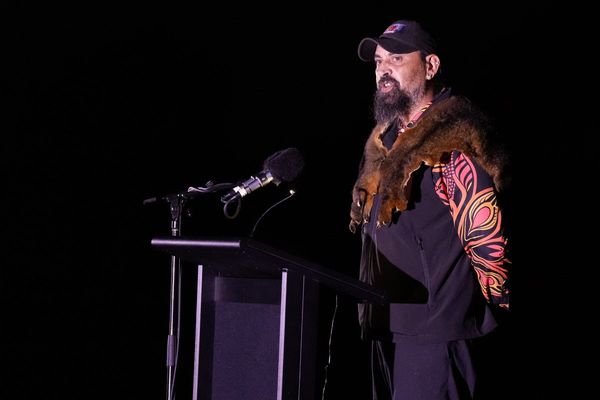
“We need to deal with vaccine hesitancy,” she told attenders at a meeting of prominent infectious diseases experts in Sydney on Thursday, held by the Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine.
“This is a new thing for us, we’ve never had this problem before and we certainly have it now. We simply can’t get people to take vaccines for Sars-CoV-2 [Covid-19] and that’s something we need to address.
“On the African continent, we do not make vaccines. That has contributed massively to the fact that we don’t have vaccines to roll out against Sars-CoV-2 and many other [diseases]. We need to deal with that as a global community.”
Until such problems are addressed, expecting more variants “is a no-brainer,” Moore said.
“Yes, we should expect more variants, unfortunately. We’re certainly going to pick up these new variants when we continue to have this high level of community spread.”

Lewin said this reality means Australians will need to accept periodically returning to public health measures such as social distancing and masks as a way of life for the foreseeable future.
“I am not saying we need masks forever, but when infections become large we need a rapid response,” she said. “We need to remove the emotion from mask-wearing. I was just in Singapore and Korea and everyone was wearing a mask and it was no big deal. Those countries were bursting with activity, but people were wearing masks all the time. We need to recognise it’s needed, just when we have surging numbers.”
Australia is also not effectively using the tools at its disposal, like vaccine boosters, and antivirals that protect the immunocompromised and elderly from becoming severely unwell and dying, she said.
“We will also get better tools, there’s no doubt about it,” she said. “We will get better vaccines. We will get better antivirals. We will see improvements in the way we manage Covid, so I don’t think it’s all doom and gloom at all.”
But the future of the pandemic is more uncertain than it seemed even months ago, she said.
“I probably would have been more confident trying to make a prediction at the end of last year about what might happen, but now it’s very hard to predict,” Lewin said.
“What is certain is Covid is not going to go away. We will have it next winter, and it will be here next year.
“We need to plan for the worst, and hope for the best.”