Over a decade ago, I was diagnosed with polycystic ovarian syndrome, better known as PCOS, a metabolic, hormonal and genetic disorder that affects 1 in 10 people with ovaries. It took nearly that long to reach the diagnosis. As a syndrome, PCOS is not discovered by a single test. In fact, it is characterized by a multitude of overlapping factors including excess facial and body hair, insulin resistance, irregular menstrual cycles, hair loss, abnormal weight gain, severe acne and infertility. In some, but not all cases — contrary to its name — PCOS can also manifest as small noncancerous ovarian cysts.
When I first told my doctor that I suspected PCOS to be the culprit for my personal journey with infertility, it was the lack of those cysts that led her to dismiss my claim. “It’s not that,” she told me. “You don’t have any cysts. You should just lose some weight, and things will work themselves out.”
Things did not work themselves out.
My menstrual cycles ranged from nonexistent to lasting literally months on end. My hair and skin were oily and brittle, with acne to rival any pubescent teen. The quest to become a mom seemed like an unattainable goal. So I did what at the time felt terrifying to me. I changed doctors and finally got a clear diagnosis, followed by an action plan. One that did ultimately include a look at my nutrition and exercise but also recognized that PCOS was causing insulin resistance and other metabolic changes that had sabotaged all my previous weight loss efforts.
My husband and I eventually underwent in vitro fertilization to conceive our son, but my journey with PCOS didn’t end with getting pregnant. Not many people’s journeys do.
A 2017 study by university researchers from Australia, Chicago and Pennsylvania, “Delayed diagnosis and a lack of information associated with dissatisfaction in women with polycystic ovary syndrome,” found that while PCOS is the most common endocrine disorder in women, many will often spend more than two years and see at least three providers before receiving a diagnosis. When I see those statistics, I see time slipping away from people who desperately deserve better. I see missed days of work from debilitating ovarian pain, increased anxiety from hormonal surges and yo-yo dieting that never works. I see lowered body image from male-pattern baldness, unwanted facial hair and never-ending acne breakouts. Yet, had I not been experiencing and blogging about infertility, I never would have learned about PCOS.
That thought haunts me because PCOS, like many other reproductive health issues, is just one branch on a tree. People with PCOS are three times more likely to develop endometrial cancer and carry twice the risk of high blood pressure, heart attack or stroke. The insulin resistance caused by PCOS leads 35% of women with PCOS to develop prediabetes. So why don’t more people know about this condition?
Well, under the umbrella of reproductive health, the more serious effects of issues such as PCOS, endometriosis and fibroid tumors get lost, leaving thousands of women and girls with pain and other symptoms that are swept under the rug until they become utterly unbearable. It almost seems to be just the mention of the term “reproductive” that somehow clouds the conversation, with people immediately thinking about sex and babies. When honestly, reproductive health has far less to do with reproduction itself than one might think, and until we stop being squeamish about discussing things that happen “down there,” people with ovaries will continue to face disproportionate care and lower quality of life.
There is no cure for PCOS, but it can be managed, and the sooner we get talking about what it is, and the various symptoms that make up the diagnosis, the more we can help others take control of it before it takes control of their lives.
September is both PCOS and Ovarian Cancer Awareness Month. I encourage you to support the nearly 6 million of us affected by PCOS or at risk for ovarian cancer by wearing teal, the national awareness color for both, and by visiting sites such as my own, thebrokenbrownegg.org, for a personal account of my journey with the syndrome, or the National Polycystic Ovary Syndrome Association’s website PCOSChallenge.org, where you can get the latest information regarding PCOS diagnosis, treatment and activism.
Reproductive health is health. Full stop. For the thousands of people affected by conditions such as these, their overall health and the equity of their care should receive far more concern than we give attention to.
____
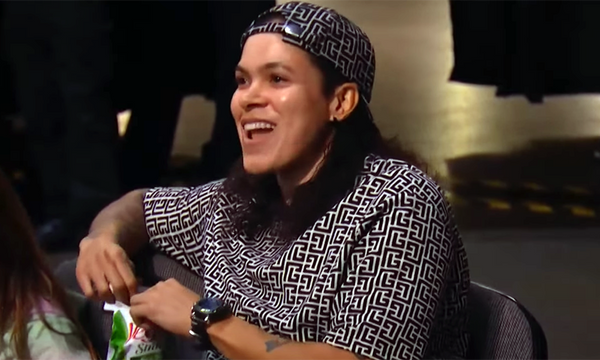
ABOUT THE WRITER
Regina Townsend is an award-winning youth librarian, infertility advocate and founder of The Broken Brown Egg, an internationally recognized reproductive health organization. Townsend recently published her first book, “Make IF Make Sense: Putting Words to the Feels of Infertility.”