In 2020, we saw windows pasted with rainbows, hospitals flooded with donations and NHS workers regularly described as heroes. While linked to heightened risks faced by health workers during the pandemic, notions of self-sacrifice in nursing are not new. In fact, they have long underpinned the very nature of the role.
With the professionalisation of care work in the 19th century, in a society where a woman’s role was defined by caregiving, nurses were considered married to the job. Like military or monastic life, nurses were expected to not only suffer hardships without complaint but embrace them as part of your life’s service.
As written by E Glover, in a letter to the Nursing Journal, published in 1903:
A good nurse can never be compensated by money, She must be paid … but her work must be something better, something higher, and I may add purer and holier than the ordinary commerce of today.

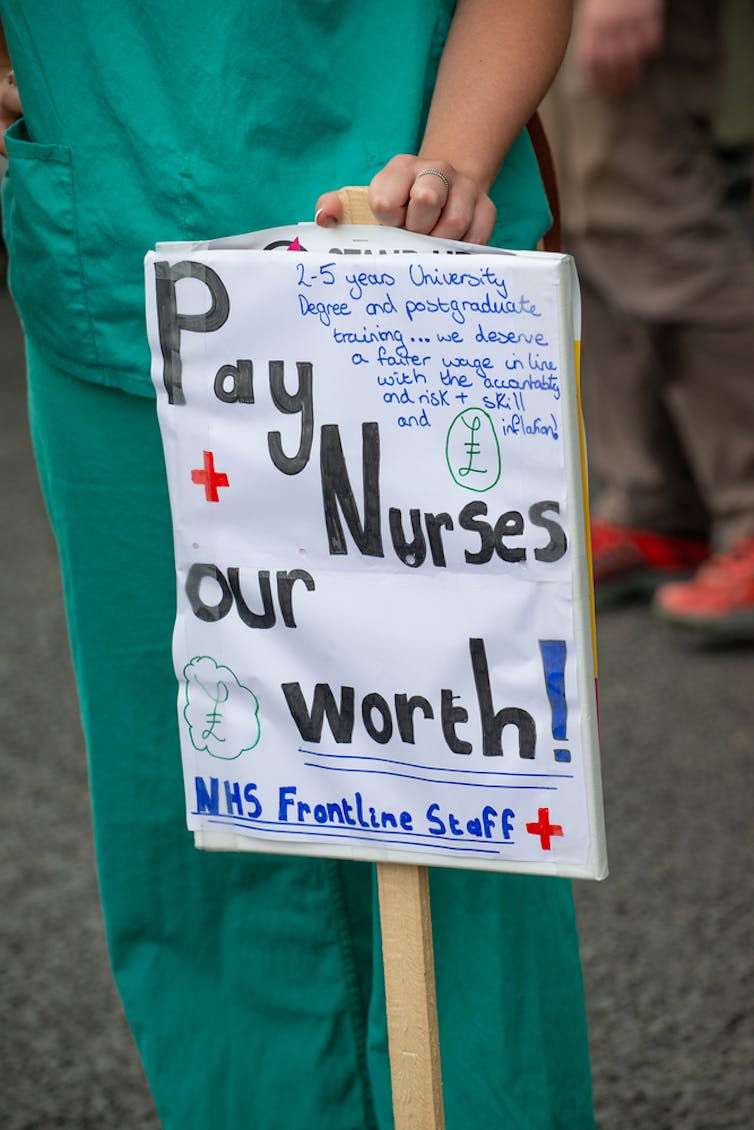
Women’s and workers’ rights have come a long way since then. Yet bedside nurses’ role, job autonomy and even salaries are still defined by the notion that, as naturally compassionate individuals, they should be willing to sacrifice parts of themselves to provide care to others.
“Bedside nursing” refers to direct patient care and includes registered, associate and assistant nurses across a range of settings. The majority work day and night shift patterns and are not paid above band six (at which level, you can earn a maximum of £39,027, once you have over five years of experience). Above that, you move into management or become a specialist practitioner.
Over my 15 years of working bedside, I have seen hundreds of ward staff experience burnout. My doctoral research into ward-based care distribution shows how bedside nurses are particularly vulnerable to distress and burnout. Such stresses are only compounded by hero narratives.
The enduring ideal of nursing as a calling
The historic division of employment by gender and class underpins a hierarchy of labour within modern healthcare systems. Despite performing the majority of patient care and being subject to the most risk, bedside nurses occupy the lowest clinical pay bands.
Medicine has long been considered a professional specialism. Nursing, conversely, was seen as a vocation. This is rooted in the idea that care work is altruistic, and that caring is a disposition – not a skill.
Following this traditional demarcation between cure and care, the continued efforts of regulators and unions to cement nursing as a skilled profession have, sadly, led to an increased devaluation of direct patient care and bedside nursing.
With diagnostic and life-promoting treatments prioritised, the fundamentals of healthcare – observation, hygiene, nutrition and comfort – are framed as the basics and, therefore, least valuable. This is defined by a pay structure that effectively rewards staff financially for moving away from bedside nursing and into a nine-to-five role, despite their having the biggest direct impact on patient care outcomes.
This divestment does not reflect either the necessity or demands of bedside nursing. It is physically and emotionally laborious work, and it comes at a price. Cross-workforce studies demonstrate that nurses across the board are unquestionably more at risk of post-traumatic stress disorder, anxiety, depression, alcohol dependency, self-harm and suicidal thinking.
While research has shown a link between increases in mental health disorders among staff and peaks in COVID admissions, this has less to do with the trauma of COVID-specific care than it does the increased adverse impacts of being overstretched and under-resourced.
This was most keenly felt beyond the COVID critical-care wards into which resources were pooled, something I witnessed firsthand.
How rationing care causes distress to patients and staff
During the first wave I was redeployed to a COVID high-dependency unit, looking after patients who were critically ill. This left me shocked, stressed and upset. But nothing prepared me for my return to a depleted and overburdened oncology ward for the second wave.
There, patients were neglected because we were unable to adequately meet their needs. It was there – and not on COVID wards – that I felt unsafe, that I witnessed more drug errors, longer wait times, inadequate levels of basic care and limited lifesaving interventions.
When need is limitless and resources are finite, patients suffer indignity, harm and neglect. How bedside nurses prioritise who gets their time and attention forms the crux of my research. I have found that the process of denying care to some in order to provide to others – which experts refer to as care “rationing– has a seriously detrimental effect on bedside nurses.

Healthcare rationing is a human rights issue and not being able to provide good care is a significant cause of distress. Unlike policy and macro-level rationing, where institutions are ultimately held responsible for the effective neglect in which the rationing results, care rationing shifts the moral responsibility to the carer.
Nurses must bear the burden of deciding who gets fed their meals while still hot, who lies in soiled sheets and who is left to die alone. To try and mitigate these injustices, they get in early and stay late. They skip meals, they work through breaks, and they burn out.
I am currently working with the International Public Policy Observatory on a rapid evidence review, demonstrating how poor mental health among NHS staff is placing an overwhelming operational burden on the service. This comes at a significant financial cost.
While statistics on nurses’ mental wellbeing and its wider impact draw much-needed attention to the subject, surveys and reporting cannot do justice to the reality of working on an understaffed, under-resourced, and overstretched acute NHS ward. They cannot adequately convey the physical, emotional, and mental stress bedside nurses endure.
As long as the role itself continues to be devalued and as long as bedside nurses are held to an impossible standard, this will not change.
On Friday June 17, The Conversation’s partner organisation, the International Public Policy Observatory, is hosting an online event to launch its rapid evidence review on NHS staff wellbeing and mental health. Speakers will include Dr Steve Boorman CBE and Professor Dame Carol Black. Sign up here for this free event.
Rebecca Williams' research work receives funding from The European Social Research Council and UCL Dean's Strategic Fund.
This article was originally published on The Conversation. Read the original article.







