Sarah Traylor's cancer diagnosis came with a cocktail of mixed emotions.
She felt shocked, then realised she was lucky it was detected early.
But she also felt a deep sense of embarrassment when she was told she had anal cancer.
Initially, she kept it secret.
Like many with the disease, she told friends and family she was being treated for colon cancer.
"The minute you use the word anal, it's one of those embarrassing words, which it shouldn't be," she said.
Now doctors are hoping to break the stigma associated with anuses, because they believe they have found a way to eradicate the dangerous cells that turn into anal cancer.
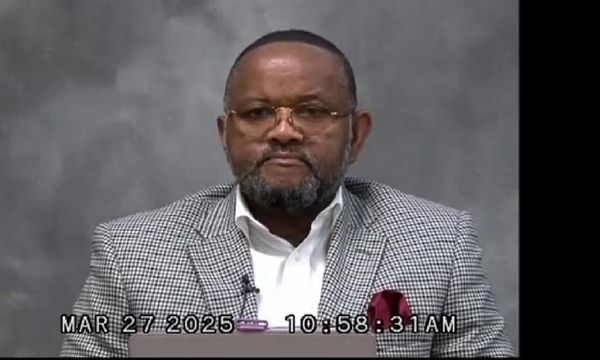
St Vincent's immunologist Richard Hillman is leading an Australian-first trial of a therapy that targets precancerous cells and the virus that causes anal cancer.
He wants more doctors to discuss anal health with their patients, so people at risk can be screened and the disease can be caught early.
"There's so much stigma associated with that part of our anatomy that people typically present very late," he said.
Promising results
Screening for precancerous cells only makes sense when there is an effective treatment for them.
Until now, dealing with this stage of anal cancer has meant regular procedures to remove lesions, with the expectation they are likely to come back.
The new therapy being trialled could make that a thing of the past.
Colorectal surgeon Hamish Urquhart has been delivering the treatment to patients at St Vincent's hospital in Darlinghurst and is pleased with how the trial is going.
"The whole idea is that it clears the high-risk lesions … and so by clearing that, we're going to prevent transformation to invasive cancer," he said.
The technique applies energy in the radiofrequency wavelengths to the affected tissue with the aim of obliterating potentially dangerous cells.
The procedure takes about 20 minutes and patients go home the day of the surgery.
Later, the doctor will follow up by using a high-resolution anoscopy to check the lesions have been removed and there has been no progression towards anal cancer.
"We're hoping we see that translate to improved cancer outcomes in six and 12 months time," Dr Urquhart said.
Professor Hillman is also confident in the results the trial is showing and thinks it could soon be possible to permanently wipe out precancerous cells detected in patients.
"I want to make anal cancer history," he said.
A similar trial in the US proved so effective at obliterating precancerous anal cancer cells, the trial had to be abandoned so all the participants, including those in the control group who were not getting the treatment, could receive the therapy.
The earlier the better
Fortunately, anal cancer is rare: of about 700 people with precancerous cells, only one will develop cancer.
In Australia, that amounts to about 500 people being diagnosed with anal cancer every year — 60 per cent of them women.
Like cervical cancer, anal cancer is caused by the highly contagious HPV virus, which can spread from other parts of the body.
In men, the disease is most prevalent among men who have sex with men, and those who are HIV positive.
But screening women who are at risk is harder.
Professor Hillman says identifying women at risk of cervical, vaginal or vulval cancer is a good place to start.
"A very simple thing we can do is offer women who've had an abnormal cervical pap in the past, just a simple self-collected swab from their bottoms," he said.
Because of the stigma, anal cancer is typically found late, which can make treatment difficult and unpleasant.
Professor Hillman and Dr Urquhart recommend people look out for a change in bowel habits, blood in their faeces, and pain, discomfort or lumps around their anus.
They say any of these signs should be discussed with a GP.
Open conversations
Jane Costello, CEO of Positive Life NSW wants more people to know what to look out for.
"We've got a lot of work to do in terms of raising awareness around anal cancer generally, but also particularly for women," she said.
"It's just not talked about."
She'd like to see GPs lead the way by opening non-judgemental discussions with their patients about anal cancer and other HPV related diseases.
"If we can make that a standard practice in medical care, then potentially we could change the way the health care system works with and for women," she said.
Ms Traylor thinks that if more doctors offered anal screening, the issue would not be so taboo and more people would be comfortable talking openly about potential risks.
She went through gruelling chemotherapy and radiation to ensure the cancer would not recur.
The treatment was successful and now she's determined to be open about having beaten anal cancer, even though she can see people are not comfortable hearing the word.
"You know that they're not because you see their reaction," she said.
"But I'm comfortable using it now."