Ryant Grant was in his 20s and serving in the military when he learned that the numbness and tingling in his hands and feet, as well as his unshakeable fatigue, were symptoms of multiple sclerosis.
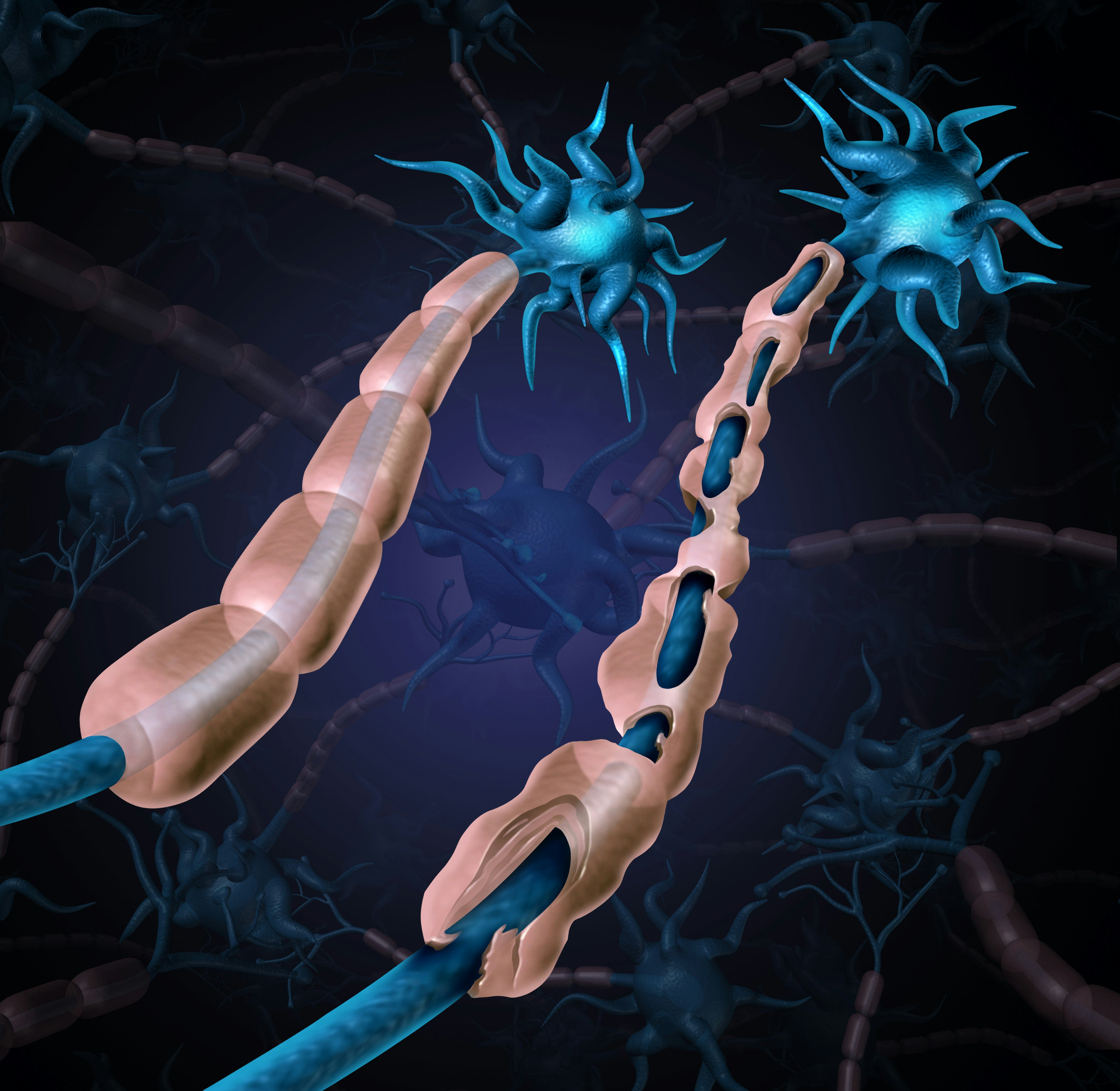
Like nearly a million other people with MS in the United States, Grant had been feeling his immune system attack his central nervous system. The insulation around his nerves was crumbling, weakening the signals between his brain and body.
The disease can have a wide range of symptoms and outcomes. Now 43, Grant has lost the ability to walk, and he has moved into a veterans’ home in Oregon so that his wife and children don’t have to be his caretakers. He’s all too familiar with the course of the illness and can name risk factors he did and didn’t share with other MS patients, three-quarters of whom are female. But until recently, he hadn’t heard that many scientists now believe the most important factor behind MS is a virus.

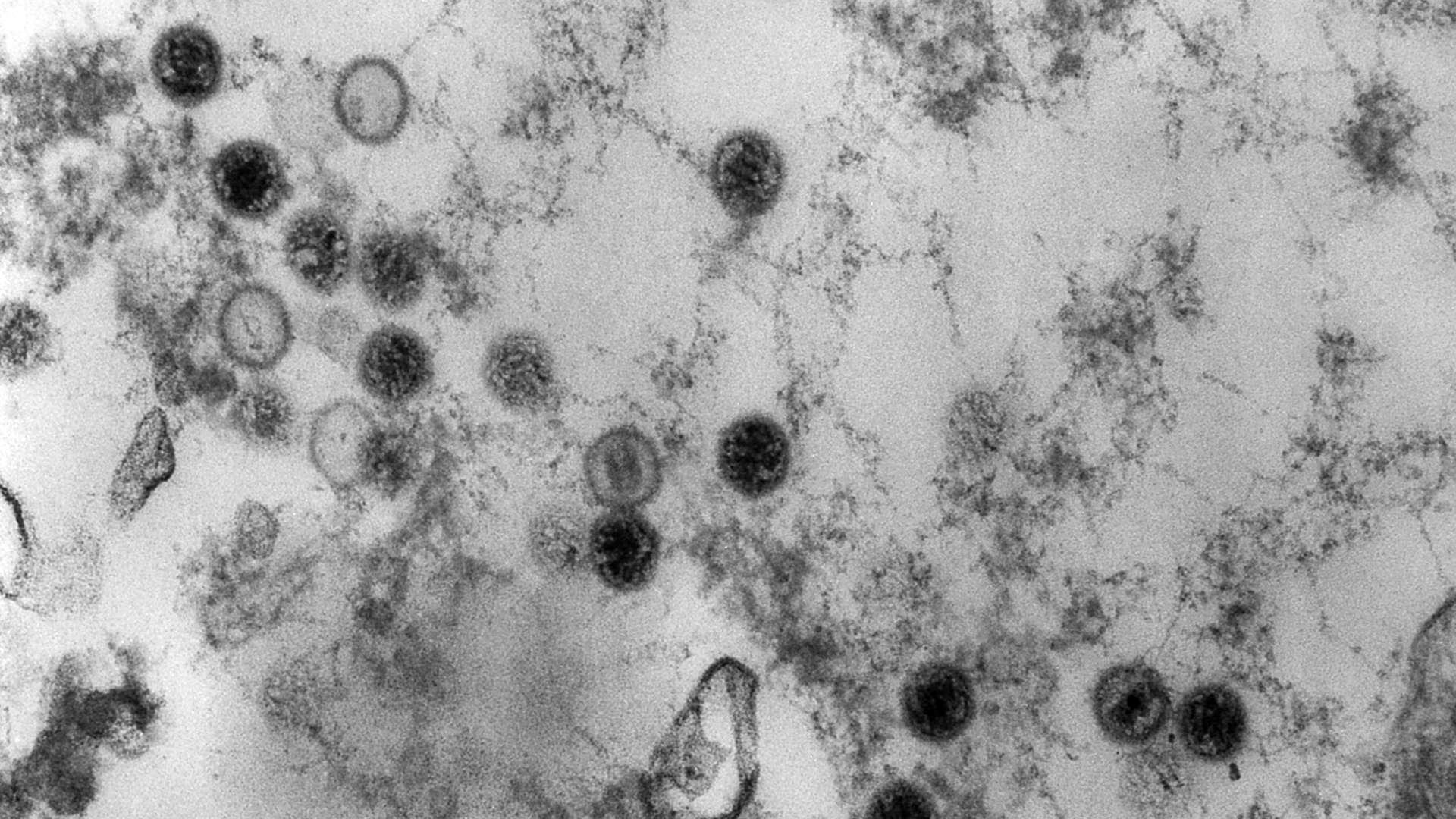
For decades, researchers suspected that the Epstein-Barr virus, a common childhood infection, is linked to multiple sclerosis. In January, the journal Science pushed that connection into headlines when it published the results of a two-decade study of people who, like Grant, have served in the military. The study’s researchers concluded that EBV infection is “the leading cause” of MS.
Bruce Bebo, executive vice president of research at the nonprofit National Multiple Sclerosis Society, which helped fund the study, said he believes the findings fall just short of proving causation. They do, however, provide “probably the strongest evidence to date of that link between EBV and MS,” he said.
Epstein-Barr virus has infected about 95 percent of adults. Yet only a tiny fraction of them will develop multiple sclerosis. Other factors are also known to affect a person’s MS risk, including genetics, low vitamin D, smoking, and childhood obesity.
“Patients often want to know why this disease happened to them.”
If this virus that infects nearly everyone on Earth causes multiple sclerosis, it does so in concert with other actors in a choreography that scientists don’t yet understand.
Amid that lingering uncertainty, scientists are discussing how to proceed from here. Antivirals or drugs that target infected cells, some of which are already in development, might help MS patients. Vaccines against EBV are in development, too. The authors of the Science paper say widespread vaccination could prevent most instances of MS. But other researchers aren’t so sure the case is closed, and they suggest putting more emphasis on understanding how the virus might interact with social factors such as stress.
“Patients often want to know why this disease happened to them,” said Lindsey Wooliscroft, a neurologist and associate director of research for the VA’s Multiple Sclerosis Center of Excellence in Portland, Oregon. “It’s frustrating when I can’t tell them.”
Piling evidence

Epstein-Barr most often strikes in early childhood, with few or no noticeable symptoms. After the initial infection, the virus lurks inside certain immune cells for the rest of a person’s life.
If someone avoids EBV until adolescence or adulthood, the virus is more likely to cause mononucleosis, an illness characterized by fever and fatigue. Mono is more common in Western countries, where kids encounter fewer germs early in life, said Alberto Ascherio, a professor of epidemiology and nutrition at the Harvard T. H. Chan School of Public Health and senior author of the Science paper.
Like mono, multiple sclerosis is most prevalent in the U.S. and parts of Europe. Scientists first suggested more than four decades ago that the two conditions might be linked. In the following years, the evidence piled up: Nearly everyone with multiple sclerosis has latent EBV in their cells. People who recall being sick with mono have a heightened risk of MS. Immune cells harboring the virus are more prevalent in the brains of MS patients.
“We’ve long suspected that Epstein-Barr virus had a role” in the development of MS, Wooliscroft said. “But it’s just been very hard to prove.”
Epstein-Barr virus has infected about 95 percent of adults. Yet only a tiny fraction of them will develop multiple sclerosis.
The surest way to prove causation would be to start with a group of healthy, uninfected adults and divide them randomly into two groups. Researchers would infect just one group with the virus and then monitor both groups afterward to see who develops MS.
In the real world, such an experiment isn’t ethical. Ascherio and his coauthors wanted to do the closest possible thing: find a group of people who hadn’t yet been infected with EBV at a given time point, then see whether those who eventually did get infected were more likely to develop MS. “Conceptually, our study is very simple,” Ascherio said. “In practice, it seemed virtually impossible to conduct.”
That’s because the scientists would need a large number of study participants to monitor over the course of years, as MS can be slow to develop and diagnose. For help, the research team turned to the U.S. military, which collects regular blood samples from active service members for HIV screening. In the end, it took two decades for the team to accrue enough data to perform its statistical analysis.
The scientists had blood samples from 801 military members who had developed MS. They matched each of those MS patients to approximately two controls without MS who had blood samples taken on the same dates. From there, the scientists looked for EBV in the blood of all the study participants.
Most of the controls already had the virus in their blood when they enrolled in the military, which wasn’t surprising. But a small percentage hadn’t been infected yet. That’s the group the scientists were most interested in. Among the initially negative people, those who contracted EBV in the following years were 32 times more likely to develop MS than people who never got the virus.
“It’s a pretty striking paper,” said Daniel Tancredi, a statistician, and professor of pediatrics at the University of California, Davis, who was not involved in the work.
“In practice, it seemed virtually impossible to conduct.”
The authors also looked at the likelihood of MS in people who had been infected with EBV at any time — before or after joining the military. This time they found the risk of MS was about 26 times higher than without an EBV infection, slightly lower than in the group infected during military service. (The result fits with previous research suggesting that people who’ve had mono — indicating an EBV infection later in life — are at higher risk of MS than people infected in early childhood.)
Ascherio’s group found an additional clue: a protein called neurofilament light chain drifting in the blood of future MS patients after they’d contracted EBV. This protein normally resides inside the sheaths that insulate the molecular wiring between neurons, helping their signals travel quickly. Its presence in the blood was a sign that the infected subjects’ nerves were already under attack.
All of the evidence is circumstantial — the virus spotted at the scene of the crime — because the imaginary experiment that would prove causation is impossible. Still, Tancredi said, the scientists have found “very strong evidence” pointing to the perpetrator.
Incomplete findings?
“The work in the Science paper was stunningly elegant. It was just terrific science,” said Ralph Horwitz, a professor of cardiovascular sciences at Temple University’s Lewis Katz School of Medicine. In a paper published this September in the Journal of Clinical Investigation, though, Horwitz and coauthors called the analysis by Ascherio’s group “incomplete” and wrote that it “misrepresents the data.”
Horwitz thinks it’s a mistake to focus only on the Epstein-Barr virus. He’s interested in what he calls biosocial medicine, which he has defined as “a comprehensive theory of medicine that integrates both the biology and biography of the individual patient.” Loneliness and social isolation, for example, have been linked to heart disease and other problems. Socioeconomic disparities are associated with worse Covid outcomes in patients who aren’t white.
When Horwitz saw the Science paper, he told Undark, it struck him that the strongest link between MS and EBV seemed to be in people who started out negative for the virus, but contracted it during their military service. He wondered whether something about military service itself — maybe deployment to a certain environment or stress and trauma — might add to a person’s risk.
He and his coauthors proposed a different way to parse the military dataset that Ascherio’s group had gathered. If you consider only people infected before joining the military, they argued, EBV infection seems to raise the risk of MS much less dramatically.
Horwitz’s group raises a “crucial question,” said Tancredi, the biostatistician. However, he said, they made an error.
To answer their question, Tancredi said, Horwitz’s group should have compared MS risk between people with past EBV infections and people who were never infected. Instead, they lumped together the never-infected subjects with a third group: those infected during military service.
“I don’t know how it got to be published.”
But because of the way Ascherio’s study was designed — the scientists started with known MS cases, then added controls — there are an artificially high number of MS cases among the later-infected adults. In a broad sample of people who contracted Epstein-Barr virus in adulthood, only a tiny number would develop MS. So in Horwitz’s comparison, according to Tancredi, the groups (those infected in childhood versus everybody else) appear to have a more similar risk than they really do.
Horwitz stands by his analysis. But Ascherio has a stronger take on the paper that argues with his own results. “Sorry to say, but that article doesn’t make any sense,” he said. “I don’t know how it got to be published.”
Still, past research has found intriguing links between stressful life events and autoimmune conditions. A study of veterans who had served in Iraq and Afghanistan, as well as a long-term study of U.S. military personnel generally, found that those diagnosed with PTSD were more prone to autoimmune conditions including multiple sclerosis, rheumatoid arthritis, and lupus. A large Swedish study also found that people with stress-related disorders were at greater risk of autoimmune conditions.
Other researchers found that MS was more common among Danish parents who had experienced the death of a child, especially if the loss was unexpected. However, a large study of female nurses found that those who reported high stress at home were no more likely to develop MS.
Regardless of the role of stress, many factors seem to contribute to whether a person develops MS. For example, “There’s a clearly a genetic piece to this puzzle, but it’s not a single gene,” said Bebo, at the National MS Society. According to Bebo, the Science paper implies that EBV is a necessary piece of that entire disease puzzle, but it’s not sufficient.
Wooliscroft said that many of her “more medically savvy” patients have asked her about the EBV connection. “I tell them that we’re still humbled by the fact that we don’t exactly know what causes MS,” she said.
Grant, the veteran, said that his doctors blamed the chemicals that he encountered while working on military helicopters. Exposure to organic solvents has been shown to increase the risk of MS, perhaps through lung inflammation. “They felt that that is what contributed most to my diagnosis,” Grant said.
He also credits being born in Montana; research has suggested that people living at higher latitudes have a greater risk of MS, perhaps because of less sunshine and lower vitamin D.
While Grant can see why stress might be part of some people’s disease stories, it doesn’t feel relevant to his own case. He was never in combat and considers himself a positive person. What was stressful, Grant said, was trying to live at home while the illness took away his mobility.
The MS puzzle
Multiple Sclerosis isn’t the only disease in which EBV has been implicated. The virus raises a person’s risk of nasopharyngeal cancer and certain lymphomas. A 2018 study found that a viral protein from EBV may activate genes that raise the risk of lupus, as well as genes linked to other autoimmune conditions. Even on its own, EBV can be reactivated in a person’s body and cause illness in adulthood.
“EBV’s a bad guy,” Wooliscroft said.
For these reasons, researchers have already been working for years to develop vaccines against EBV. Bebo said the new evidence more strongly linking the virus to MS “just adds more urgency.” There are also drugs in development that aim to treat MS by targeting the cells where latent EBV is hiding.
Horwitz, though, points out that vaccines have costs and potential side effects. He thinks that scientists should first try to better understand how social factors combine with biological ones to produce MS and other illnesses.
With that knowledge, “we can begin to unravel the mystery of a lot of diseases that create a high degree of disability in our population,” Horwitz said. “We need to understand this interplay of biology and biography better before we think about going out and vaccinating the entire population.”
Although nearly everyone in the world gets infected with EBV, multiple sclerosis is rare.
“There’s clearly a genetic piece to this puzzle, but it’s not a single gene.”
Ascherio doesn’t think this is an argument against EBV as the most important culprit, or against vaccination. “It’s very typical of viruses to cause severe disease in only a few infected individuals,” he said. He estimates EBV causes MS in about 1 in 200 individuals, similar to the rate of paralysis in people infected with polio.
“In all diseases, you have a combination of risk factors,” Ascherio said.
If other genetic and environmental factors need to come together with EBV to produce MS, what does it really mean to say that the virus causes the illness? According to Ascherio, “it means that if you eliminate the virus, you don’t get the disease.”
Grant said that knowing exactly what caused his own disease wouldn’t change much for him. He’s more focused on trying activities to maintain the mobility he still has, such as learning to play the keyboard.
Even so, he said, “I mean, it would answer that question that you have in the back of your head: Well, why did this happen to me?”
This article was originally published on Undark by Elizabeth Preston. Read the original article here.







