An asthma sufferer endured an ‘horrendous’ 10-hour wait in A&E after falling ill and having breathing difficulties. Dave Moth, 30, from Middleton spent a night on a ‘rock hard’ floor at Royal Oldham Hospital, with staff offering no indication of when he would be seen or where he could get a drink of water or find a vending machine, his partner Becka Jackson claims.
Becka, a transport manager, had called the NHS 111 helpline after he became feverish one evening at the couple’s home in Boarshaw. She is now calling for health bosses to make changes to take the pressure off A&E departments, believing a ‘massive’ update to the 111 service or more ‘face-to-face’ GP appointments could take the pressure off urgent and emergency care.
“If anyone said ‘I’m going to A&E in Oldham, I would say ‘don’t bother’ - one guy had been sat in a bed in a corridor for 20 hours,” she told the Local Democracy Reporting Service. “Yes, the NHS is free. Yes, we are very lucky. But, you know what, if I was that poorly I thought I’d die, I'd much rather be at home than lay on a bed in a corridor for 20 hours."
READ MORE : Rochdale Infirmary's emergency care changes - here's everything you need to know
The 30-year-old called 111 at around 9pm on Tuesday, June 7 and, after answering a series of questions that she describes as 'vague', was told an out-of-hours doctor would call her back within six hours.
To her relief, she received a call just 40 minutes later - but was left frustrated when the doctor began asking the same questions she had previously answered and found his insistence on speaking to Dave ‘really rude’. "I said ‘If you listen, you can hear him being sick at the side of me'," Becka said.
The couple were advised to go to A&E at Royal Oldham Hospital. On arriving at A&E just before 11pm, they reported to reception - and were asked the same questions as the 111 service and out-of-hours doctor, Becka says.
“I said, ‘I’ve asked these same questions twice, he can’t breathe, I don’t know what more you want to know’,” said Rebecca. She said Dave, an HGV mechanic, was given a card to take into a corridor where some initial medical checks are done.
However, she says there was then ‘no communication whatsoever’ for patients, who were given little reassurance or information. “ People are sat around, nobody knows where they are going because it’s not signposted very well,” she added.
“Once the checks are done you go and sit in a waiting room. One woman, quite an elderly lady, had been there six hours. She was in her pyjamas and in a lot of pain. As we got there, there were 10 ambulances outside A&E - I went back to my car and there was a queue of beds all the way down the corridor.”
Becka feels the issues are not the fault of doctors, nurses or receptionists - but points the finger at ‘power mad people who look at spreadsheets and not the real world’. But she feels the situation she and Dave were faced with at A&E was unacceptable and needs to be urgently addressed.
“People left without a drink of water for hours,” she said: “There was one vending machine that was out of order. There were no staff saying ‘go through this corridor to this vending machine’. There was no communication whatsoever.”
A water spillage was also left on the floor for five hours, Becka said. She continued: “I was sat on one seat, my fella was on the floor asleep. The seats are rock hard so I got on the floor and he got on the seat. It felt like no one knew what was going on. I know it was busy, but if they had said it’s a 10-hour wait then we can decide if you can ride it out or should go home and go to the doctor first thing in the morning.”
Following an arduous night, Becka - who describes the whole experience as ‘horrendous’ - was further angered when someone arrived in the morning and was seen after just one hour. After complaining, she was told that a doctor was looking at Dave’s notes.
Again she found the communication and reassurance lacking - describing how doctors were sometimes stepping over patients on the floor and ‘were huffing and puffing’ when people took time to gather themselves when they were eventually seen.
A further frustration was seeing people leaving, having been told to take over-the-counter remedies such as paracetamol, Ibuprofen and Gaviscon - and in one case told to rest.
To Becka this suggests ‘either 111 needs a massive update on questions they ask and where to send people, or doctors need to open face-to-face appointments up’. "You can’t expect people to be in A&E and no one talking to you," she said. "There’s just nothing, you just sit there in silence, the doctor stepping over you while you are asleep on the floor.
"It’s not the staff’s fault, they are under a lot of pressure, but something needs to change, because it’s really not going in the right direction. I don’t know what the solution is, but there’s got to be something.”
Dave was finally seen by a doctor at 8.30am - nearly 10 hours after arriving at A&E. He was diagnosed with a throat infection which had triggered an asthma attack. He said he would also need anti-sickness tablets, but was told he could get these over-the-counter.
However, this was not the case and this resulted in yet another delay, with Mr Dave’s GP having to write a prescription for collection from his local pharmacy.
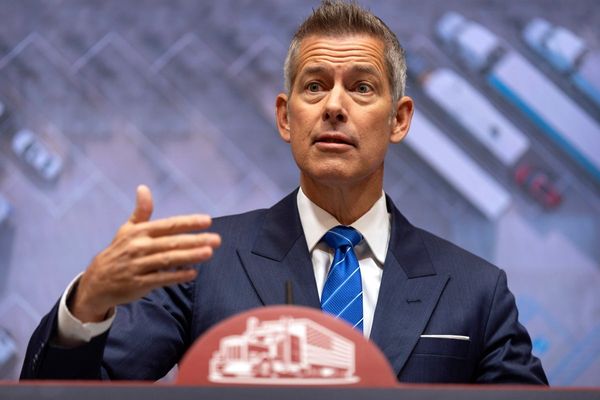
David Jago, Chief Officer for Oldham Care Organisation, which runs The Royal Oldham Hospital, has responded to Rebecca’s concerns over A&E. He said: “Like many A&Es across the country, we have seen a steep rise in the number of patients accessing our services, which is putting additional pressure on staff and causing some unavoidable waits.
"The safety of our patients is our first priority and patients are seen in order of clinical need. We apologise for anyone who has waited for treatment or had a poor experience during one of our busier periods and would encourage people to get in touch with our PALs team to discuss any aspect of the care they received they are not happy with.
“We’d urge everyone to help us by accessing the right services at the right time. A&E is for urgent and life threatening emergencies. We would encourage you to phone NHS 111 for advice on treatment if you’re not sure where to go.”
Heywood, Rochdale and Middleton Care Commissioning Group, who commission the 111 service in the area, declined to comment.
READ NEXT :
- This is the polio vaccine uptake in Greater Manchester as 'national incident' declared
- More than quarter of a million Greater Manchester women miss their cervical cancer screenings - why it's important, according to experts
- Nurse shortage forces closure of minor injuries unit for at least another five weeks
- Engineer fears he will lose hand after agonising saw accident as operations cancelled twice
- Before-and-after-school club hailed by inspectors for raising its game