
On Sept. 3, 1973, a fire swept through the baghouse of the Bunker Hill mine in Idaho’s Silver Valley. The building was designed to filter pollutants produced by smelting, the melting of rocks that separates metal from its ore. The gases produced in this process carried poisons, including lead.
At the time, the prices of lead and silver were climbing toward all-time highs. Rather than wait for new filters and repairs, company officials kept the mine running. They increased production, bypassed the filtration steps and, for eleven months, dumped noxious gases directly into the surrounding area.
Then, horses in the area began dying.
When data on children’s blood lead levels began to arrive in September 1974, one year after the fire, the results were shocking. The fire became one of the largest single lead-poisoning events in U.S. history.

Without filters, the mine operations deposited an estimated 35 tons of lead per month in the area, four times more than before the fire. Between January and September 1974, it also released more than 2 tons of arsenic and 2.5 tons of mercury, among other metals and toxic chemicals, according to data collected by Restoration Partnership.
Lead still contaminates the soil across Silver Valley today, and it continues to wash down tributaries and into the Coeur d’Alene River and Lake Coeur d’Alene. Many people in this fast-growing region are unaware of the risks.
How lead harms human health
Our bodies use metals like zinc, iron and calcium. However, we have zero need for lead. Its chemical composition makes it both highly toxic and able to infiltrate almost every organ in the body.
Lead exposure can cause high blood pressure and cardiac disease. It can also cause problems with brain development, kidney function and reproductive health, including miscarriages, prematurity and low birth weight. Children are especially susceptible to lead’s toxic effect on the central nervous system; they absorb it up to 17 times more readily than adults, and their brains are still developing.
The Centers for Disease Control and Prevention’s reference value for levels of lead in blood has changed as knowledge about this potent neurotoxin has evolved. In 1973, a blood lead level of less than 40 micrograms per deciliter in children was vaguely defined as “undue lead absorption.” In 1991, anything above 10 micrograms per deciliter was considered a “level of concern.”
Today, 3.5 micrograms per deciliter is the reference value, meant to identify the 2.5% of children with the highest blood lead levels. The CDC no longer uses “level of concern” as a threshold, because there is no safe blood lead level in children.
Children’s health after the Baghouse Fire
The children of the Silver Valley were exposed to extremely high levels of poisons after the Baghouse Fire at the Bunker Hill mine.
Ninety-nine percent of children within a mile of the smelter who were tested after the fire – 173 out of 175 kids – had blood lead levels of 40 micrograms per deciliter or higher. Their average blood lead level was 67.4 micrograms per deciliter. A 1-year-old tested at 164 micrograms per deciliter, the highest ever recorded in a child.
Cognitive impairment in children, as measured by loss of IQ points, can occur at levels of less than 5 micrograms per deciliter.
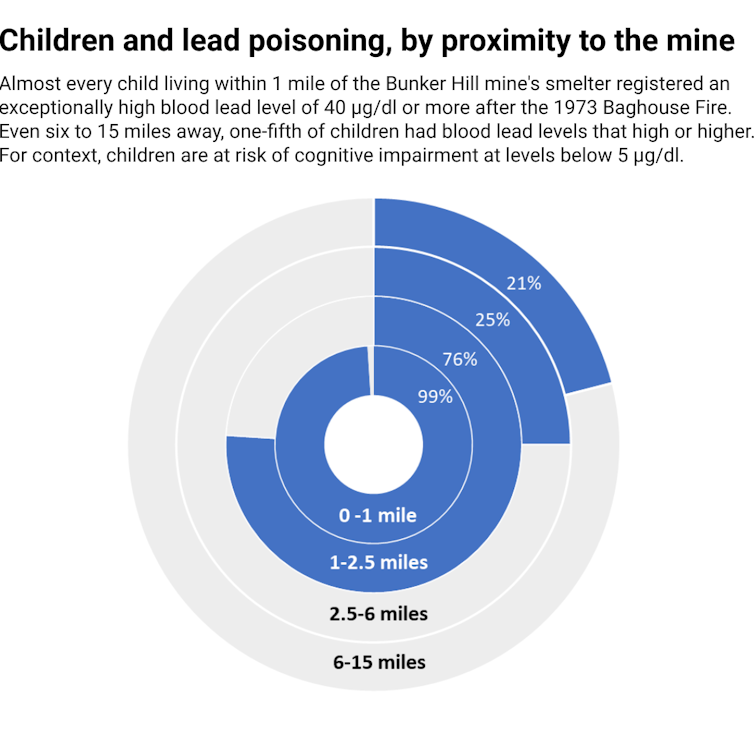
To put the Silver Valley numbers into context, the average blood lead level for children in Flint, Michigan, at the height of the lead-pipe water crisis in 2015 was 1.3 micrograms per deciliter, and 21 children had blood lead levels over 10 micrograms per deciliter.
It is difficult to assess the extent of the damage from the Baghouse Fire in the children of the Silver Valley. Doctors in the 1970s weren’t able to test for cognitive and neurologic problems in the most vulnerable children, birth to 3 years old. Michael C. Mix describes in “Leaded: The Poisoning of Idaho’s Silver Valley” how the politically powerful company that owned the mine also suppressed and distorted health findings. Blood lead levels in children in the area remained higher than 40 micrograms per deciliter into 1980.
Continuing health risk in Silver Valley
The legacy of the Baghouse Fire continues to haunt Silver Valley, but that incident 50 years ago is only part of the picture. Decades of contamination from other mines in the area poses further risks.
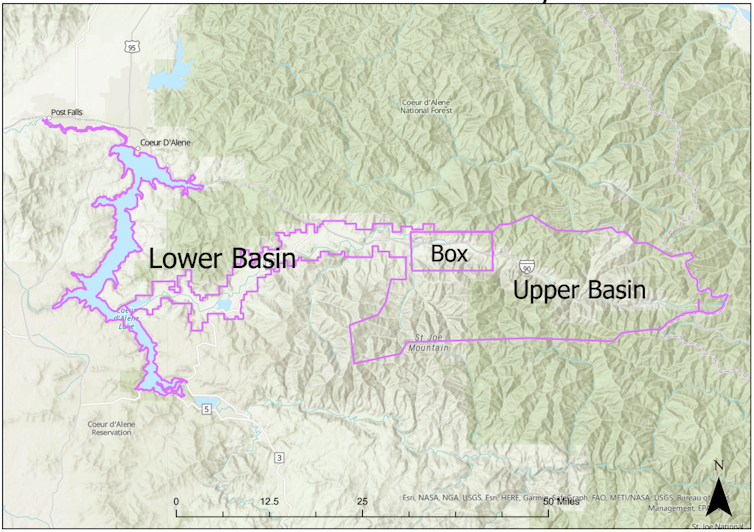
At its height, the Silver Valley area had over 200 active mines. Today, it is the largest contiguous Superfund site in the nation – 1,500 square miles (3,885 square kilometers) across northern Idaho and eastern Washington. Multiple agencies, including the U.S. Environmental Protection Agency, Idaho Department of Environmental Quality, Panhandle Health District, the Coeur d’Alene Trust and the Coeur d’Alene Tribe (Schitsu’umsh), are active in monitoring and cleanup operations.
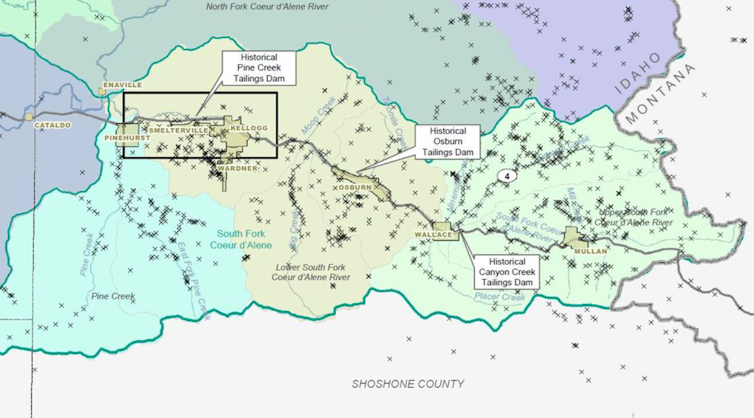
Early efforts to clean up contamination from the fire concentrated on residential areas in “The Box,” a 21-square-mile area (54 square kilometers) around the old smelter site and the towns of Kellogg, Smelterville and Pinehurst. Workers dug up contaminated earth and removed it, and officials monitored the environment and human health.
The cleanup today is much more extensive and ongoing, with efforts focused on cleaning up the old mine and mill sites and recreational areas.
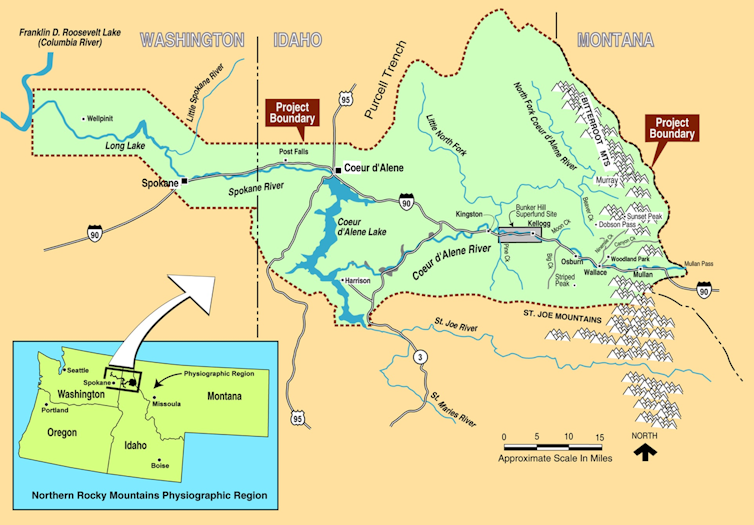
Lead does not biodegrade. It’s in the soil, along waterways and even visible in sediment to the naked eye. It is estimated that the Coeur d’Alene River delivers about 200 tons of lead to Lake Coeur d’Alene every year.
Swan deaths show the continuing risk
Blood lead levels in the area have come down dramatically since 1973, but they are still concerning. In 2022, the average blood lead level for children in “The Box” was estimated at 2.3 micrograms per deciliter, above the U.S. average. The average for the surrounding area was higher, 3.3 micrograms per deciliter.

Lead also affects area wildlife. Over 95% of wetlands in the Lower Basin contain sediment that is toxic to wildlife. Tundra swans, whose eating habits make them very susceptible to heavy metal poisoning, are a recent casualty. For these migratory birds, the area is a stopover. Since 2008, average swan deaths are estimated at 50 to 60 birds per year. There were over 300 bird deaths documented in 2022; a study is underway into the cause.
To complicate matters, many local residents have forgotten or never learned about the Baghouse Fire and the environmental issues associated with the site. Others choose to simply disbelieve the harmfulness of lead.
As Idaho’s population booms, people aren’t aware
Today, Idaho is one of the fastest-growing states in the U.S., with an influx of new residents oblivious to the local history and unaware of the threat that lurks below their feet and in the beaches of the beautiful lakes and rivers in the area. With population growth comes development, digging and disturbing contaminated soil.
Even normal weather conditions – from dry windy days that stir up lead dust particles to heavy rainfalls that mobilize contaminated sediments – can have detrimental effects on human health and on the environment.

Health risks remain, particularly along the banks and shores of the South Fork and the main Coeur d’Alene River, which are now popular recreation areas. Advisories about the lead risk in fish are still common, even downstream in Spokane, Washington.
Children and pregnant women are the most vulnerable; lead crosses the placenta, and it is present in breast milk. Major outreach efforts are underway to educate those living, working or visiting the area.
Idaho’s Panhandle Health District offers free lead screenings year-round to anyone living or spending time in the area. In-home follow-ups are offered to those found to have elevated lead levels. Meanwhile, the cleanup, which started in 1986, will continue for decades to come.
Mary Rehnborg, program manager for the Institutional Controls Program in the Panhandle Health District, contributed to this article.
Martin Schiavenato does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
This article was originally published on The Conversation. Read the original article.







