People with motor neurone disease have spoken of their devastation over the likely loss of access to a life-extending drug due to an NHS cost threshold that has not been raised since 2004.
Tofersen has slowed the progress of the illness in trials, but the chances of the drug being recommended for use in England and Wales are said to be slim.
The National Institute for Health and Care Excellence (Nice) applies a “cost-effectiveness” threshold of up to £30,000 for a drug that gives a patient a year of good-quality life, known as a Qaly.
The figure was set in 2004 and has not changed despite studies showing that the threshold would today be closer to £50,000 if it had increased in line with inflation.
Tofersen, made by the pharmaceutical company Biogen, is expensive because it is a genetic therapy administered by monthly lumbar puncture and requires short spells in hospital.
The drug would be targeted to help the 2% of those with MND who have alterations in the SOD1 gene – the equivalent of 100 people in England and Wales.
MND patients had hoped that Tofersen would be assessed as a treatment for an extremely rare condition for which there is a £100,000 threshold.
Nice is basing its assessment on the lower figure as it does not regard the alterations in the SOD1 gene as being clinically distinct from amyotrophic lateral sclerosis, the most common form of MND. The NHS is legally obliged to provide medicines recommended by Nice.
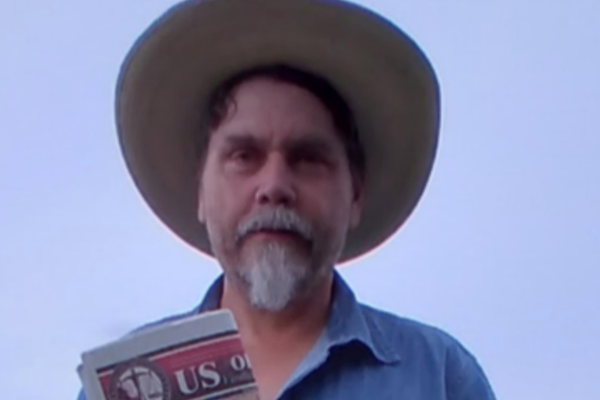
Mike Thomas, 59, from Bridgend, was diagnosed with MND four years ago. He has been on Tofersen since June last year as part of a trial and improvements in his condition have ranged from a greater capacity to walk to more energy.
He said: “It has been proven to be effective and I would be devastated if treatment ended. Tofersen is a source of hope. I saw all the publicity when the trial was concluded about the promising results.
“I try to be realistic and keep a lid on my expectations but, in my heart, I’m hoping not only for an end to disease progression but an improvement in symptoms.
“Tofersen could be snatched away as Biogen said they would continue to provide the drug until Nice make a decision. This decision could be taking away our one chance of recovery and long-term survival.”
Prof Ammar Al-Chalabi, a researcher in neurology and complex disease genetics at King’s College London, said he was concerned that Biogen would give up on seeking market authorisation. He said: “There’s a risk that the company might not want to go through the effort of putting it to market assessment and then no one will have it because they’ll say, ‘Well, there’s no way it will be approved with that Qaly level of £20,000 to £30,000.’”
Al-Chalabi said it was “crazy” that the lower cost-effectiveness threshold had not been raised over the last two decades as the purchasing power of the pound had declined.
“It should [also] be higher for this particular treatment because it’s a rare condition,” he said. “It requires precision medicine. Precision medicines are going to be expensive because they’re more difficult to develop.
“And if Britain wants to be at the forefront, which it currently is in biotechnology in the world, you have to be attractive to pharmaceutical companies for exactly these sorts of therapies.
“We’re not in a kind of blunderbuss approach. We’re in a targeted medical approach. So you want to appeal to companies to carry on doing that – that’s the only way we’re going to cure some of these diseases.”
Tanya Curry, the chief executive of the MND Association, called for an urgent review of the threshold. She said: “It’s appalling that people with a particular genetic subtype of motor neurone disease face being denied what could be a life-changing treatment because of the NHS’s outdated systems for approving new medicine.
“I would like to see an urgent review of the cost threshold Nice uses to judge whether new drugs should be approved for the NHS. It has been stuck in the same place for 20 years, indifferent to the increases in price of medicines, and has become an increasingly damaging barrier to getting innovative treatments to patients.”
Nice said cost was not the sole basis for its recommendations. A spokesperson said: “Since 2000, 84% of Nice’s technology appraisals have resulted in a positive decision – either recommended, an optimised recommendation, or referral into the cancer drugs fund or ‘use in research’.
“The figures for cancer drugs have risen significantly since the introduction of the cancer drugs fund in 2016. Only a small number of drugs receive a negative recommendation.
“Our approach allows us to focus on the topics that have the biggest impact on improving health and care outcomes and allows us to offer flexibility when appraising drugs which treat severe conditions. It is important to note that consideration of the cost-effectiveness of a technology is a necessary, but not the sole, basis for decision-making.”
A spokesperson for the Department of Health said the threshold would remain the same in 2024. She said: “It is vital we have this system to ensure spend on new medicines does not displace spending on other, more effective services and treatments.”